Webinar with Ken Price – My Unusual and Successful Treatment for my Spasmodic Torticollis (ST)
December 2021
The following is an update of a column I wrote for the Spring 2015 issue of the ST Quarterly on my unusual and successful treatment for my Spasmodic Torticollis (ST). Although I still have muscle spasms in my cervical region, they are generally quite mild and painless, I have free movement and correct posture, and the spasms often disappear for much of the day. The treatment still works as it did when I first reported on it because the root cause of the spasms had been identified and successfully addressed with surgery. In addition to the surgery, several ways have been identified that temporarily suppress spasms whenever they become annoying.
I still don’t know how common this treatment will work for other STers. We at NSTA know of two ST patients that had the same surgery as I did for conventional reasons unrelated to ST, and, to their surprise, both obtained significant improvement in their ST. I often describe my experience and treatment in support group meetings, but thus far have not found anyone in these meetings with the characteristic symptoms of my case.
Although there is no guarantee this will be of help to anyone else, I want to share in the hope a few others will find some relief. Justin Aquines suggested we hold a Zoom webinar on this, so we have planned one for Saturday, January 15, 2022 at 1:00 p.m. Pacific Time. All of my experiences in treating ST will be covered and there will be time for questions.
In this column, I will first give a history of my experience with ST leading up to the treatment. Next, I will describe what I think is happening in the medical sense. Bear in mind that I am a patient with no training or experience in medicine, so take all of this with a grain of salt. In the webinar, I’ll describe what you could look for in your case to see if anything matches my case. If so, there are some simple self-tests you can do to help decide whether to pursue further efforts through your doctor.
Background
I can remember ST symptoms starting way back in 1965 when I was in high school. One muscle in my left neck would not quite fully relax, but the spasm was not powerful enough to alter my posture, affect head movement, or create pain. I thought it was a somewhat minor, persistent sports injury and expected it to go away with time, so I did not seek treatment. As the years went by, the spasm slowly got worse, but I became used to it.
In 1976, after I completed high school and college and was several years into my engineering career, the ST symptoms went out of control and I realized I had a serious problem. My primary care doctor at that time recognized the condition as neuromuscular, but did not know the diagnosis. After much examination and further testing by several specialists did not lead to a diagnosis, my doctor sent me to a physician, Dr. David Rubin, that specialized in patients with difficult to treat muscle problems. This doctor did not give me a diagnosis, either, but he taught me a variety of exercises that restored a significant degree of muscle control over the next year. These exercises were my first big break in learning how to deal with ST.
I used these muscle stretching and relaxation techniques to provide some control over ST for the next two decades and continued seeking a diagnosis and treatment without success.
In 1997 I came across a volume describing many rare diseases put out by the National Organization for Rare Diseases (NORD) and went through it looking for something that matched my condition. I found entries on ST and dystonia and realized that I probably had ST (aka cervical dystonia, CD). This was my second break in learning about ST.
The NORD articles also provided references where additional information about ST could be obtained. This is where I found the NSTA and the Dystonia Medical Research Foundation (DMRF), among other sources. Since the NSTA office was only a few miles south of where I lived, I called and Justin answered. I explained that I probably had ST and asked if they needed volunteers. He enthusiastically accepted and here we are over 20 years later still helping those with ST.
Sensory Tricks
There was one thing I learned in the reference material I obtained from NSTA, DMRF, and the National Institutes of Health that led to my almost complete recovery. This was the phenomenon known as “Sensory Tricks” and I set about finding one that worked on me. This constitutes my third big break.
Since my engineering education and experience included working knowledge of feedback control systems, I recognized sensory tricks as mechanisms that access and influence the body’s neuromuscular control system. As explained in the following, understanding the key elements of a control system enabled me to think about what sensory tricks were doing and gave me hope that if I could find one, I might be able to exploit it and improve how it worked.
Over the next three years I found two seemingly different tricks. Interestingly, both produced an identical response by easing spasms and relieving pain. I’ll describe the tricks in the webinar to save space here. After comparing the two tricks for a couple years, I discovered they both worked because they caused a spontaneous relaxation of the muscles in the center-left side of my face. Thus, the two tricks were reduced to one simpler trick – keeping the muscles on the left side of my face relaxed. Since these muscles were not part of my ST (only left side neck and upper trapezius muscles were in persistent spasm), I had control and could maintain them in a very relaxed state. So my search at this point was to find out how relaxing facial muscles would in turn relax cervical muscles???
Since I wanted to keep those facial muscles relaxed as much as possible, I experimented with common over-the-counter topical analgesics such as AspercremeTM. The idea was to deaden the nerves that control the muscles so that they would be less likely to tense up during the day. This helped, so applying topical analgesic to the skin over the left-center part of my face became a daily routine.
Over the next two years, I noticed something a bit surprising. When in a rush to apply the analgesic, some would get on the left side of my nose. When that happened, I would just rub it in along with the other part of my face. Eventually, I noticed that when analgesic got onto my nose, the ST spasms were somewhat milder than when it didn’t. This is an example of what I was looking for: Some phenomena that beneficially influenced my ST. The effect was minor, so it took a while to notice it, but it was real and consistent. I think of this as my fourth big break because it led to the treatment that has nearly reversed my ST.
Since there are no muscles on the side of the nose, I wondered what the effect could be on ST? Keeping the facial muscles relaxed was the basis of the sensory trick, but what was the effect of the analgesic on my nose where there are no muscles? Could the act of deadening nerves in a specific location also be a sensory trick?
After thinking about this, the engineer in me decided to run a test. I started applying analgesic to the inside surface of my left nostril as well as the outside. After a few weeks of this, I was convinced that this also improved ST spasms in a small way.
Eureka
It was now 2006 and I was close to the real breakthrough. My next thought was to apply the analgesic deeper into my left nostril. For this, I had to use a Q-Tip. I studied nasal anatomy and carefully practiced applying analgesic a little deeper every day. After a couple weeks, I was applying analgesic at about the length of the Q-Tip into the nose. At this depth within the nose, the analgesic produced a dramatic effect on ST and I knew without question that I found something important. This was my fifth big break.
I then described what I found to my primary care doctor. He suggested getting an evaluation from an Ear, Nose, & Throat (ENT) physician to see if there was any obvious problem.
I made an appointment with one of the ENTs on staff in my doctor’s group, Dr. Julia Tian, and explained to her what I found. She examined my nasal passages and noticed my septum, the bone separating left and right nasal passages, was displaced to the left. I was not aware of this because it did not interfere with breathing, but Dr. Tian knew that this condition could pinch and damage a nerve passing through the area and cause severe headaches and facial pain. She had never heard of dystonia or ST, but had treated a number of patients with neuropathic facial pain caused by the damaged nerve. Treatment was fairly simple – Day surgery to realign the septum.
This was quite stunning because along with my ST I also had persistent problems with facial pain. I initially interpreted the pain as headaches, but eventually realized they were part of my neuromuscular problem. The severity of the facial pain correlated quite well with strength of muscle spasms but was curiously separate from them. The muscle spasms in my neck did not seem to directly cause the facial pain because of the separation between neck and the areas of pain. There were no spasms anywhere on my head above the neck, but the exercises and sensory tricks I did that induced muscle relaxation in the neck would also help relieve facial pain.
I did not sign up for the surgery right away because even if Dr. Tian was right about the nasal nerve being the cause of facial pain, we did not know what the connection to ST might be. I was concerned that if I had the simple surgery for facial pain, the treatment could aggravate my ST instead of easing it.
So again, being a nerdy, inquisitive engineer, I proceeded to test myself to see if I could find evidence that the nasal surgery held a real chance to treat the ST. I found several ways to shift nasal tissue away from the septal bone and each of these ways induced a prompt relaxation of ST symptoms and facial pain. Since moving deep nasal tissue away from the septum (i.e., shifting tissue further to the left) relieved pressure on the nerve, I concluded that realigning the septal bone toward the right would do the same thing and I could get some real relief from both ST and facial pain.
With this, I took the chance and scheduled the nasal surgery. When I awoke from the anesthetic following surgery, I was amazed to discover my ST spasms were greatly reduced and the persistent facial pain was all but gone. The root cause of my ST is simply the damaged and irritated nerve in the left side nasal passage. The sensory trick of relaxing my facial muscles minimized pinching of the nerve. Application of analgesic to the outside and deep inside of my nose attenuated nerve signals being sent to my brain. So both muscle relaxation and nerve desensitization with analgesic were working to reduce ST symptoms and pain.
I have provided this rather lengthy description of my experiences with ST for two reasons. First, you can see how difficult it is to find the source of the problem causing a case of ST. It was about 40 years between the time I first sensed persistent muscle spasm to the point where I understood what caused them and obtained effective treatment. The root problem with the nasal nerve was missed because it did not present any symptom that would indicate a problem. I had to find it via a very circuitous route and I had to be very lucky to read about and discover the sensory tricks that led the way. Support from the NSTA and ST patients that I met along the way also gave me great hope that a treatment could be found.
Because of this level of difficulty in finding relief, I sense the challenge physicians and medical researchers have in addressing something as complex as dystonia. I suspect there are many different causes of dystonia. Consequently, finding and treating each one is a very difficult undertaking. We can all be grateful that with the work that has been done, we now have very good generalized treatments like botulin toxins and deep brain stimulation.
Second, I hope the details in my history with ST will ring a bell with some of you and perhaps we can identify others with my condition.
In the following, I will explain what I think is happening to cause the ST. This explanation comes from the basic concepts of engineered feedback control systems. That may sound a bit far out, but I will explain in a way that you should readily see how some cases of ST develop and how it may be possible to treat them.
A Way to Think About Dystonia
As I mentioned above, I use my engineering background when thinking about ST and dystonia in general. Our neuromuscular systems are fantastically complex feedback control systems constructed from biological elements. It is useful to make a simple analogy between these physical marvels with far simpler man-made control systems.
A basic diagram of a control loop is shown in Figure 1. Action starts at the left side, where some desired “intention” is initiated. In ST patients, this could be the desire for a natural, upright posture and smooth controllable movement when desired. The brain then takes this desire and compares it to the current posture information it receives from sensory nerves throughout the body. The sensory nerve signals are “feedback” and the difference between intended and actual posture is called an “error” signal.
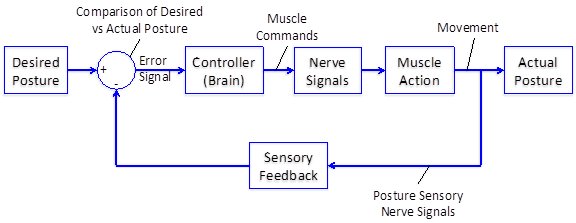
Figure 1 – A simple control loop diagram
The brain then uses this error signal to determine what the body’s muscles must do to align actual posture with desired posture. This part of the brain is the equivalent of a computer in a modern control system. In a properly functioning system, the brain always works to reduce the “error” signal to zero and place the body into whatever form is desired, whether it is posture, walking, talking, holding a fork, dancing, or swinging a baseball bat. In dystonia patients, this goal is not achieved in some part of the body, or, in some cases, even in the whole body.
Next, the brain sends out signals via muscle control nerves to adjust muscle action as required to bring posture to the desired state. When muscles receive these outbound signals from the brain, they increase or decrease their tension to reposition the body to the desired posture. Muscles are, of course, the body’s motors that activate motion and hold posture steady when the desired position is achieved.
The body’s sensory nerves detect what the body is doing at any given moment. These sensations are continuously sent as feedback back into the brain to update the error signal. You are aware of some of the sensory signals, but others are working at the subconscious level and you are not aware of them.
The whole process described above occurs continuously and when operating correctly the body produces smooth movements to accomplish that which we wish to do.
Some part of this system is not working correctly in dystonia patients. It is my understanding that medical science does not yet know for sure where or why the control system fails. A great deal has been discovered about the influence of genetic characteristics, such as the DYT1 gene mutation causing general dystonia among Ashkenazi Jews, but what that gene does is not well understood. Since many cases of dystonia arise following an injury, it is likely that sensory nerve damage may be involved in some cases independent of genetics.
We are fortunate that even within the limited understanding of dystonia that a number of effective treatments have been developed to alleviate the condition. Let’s look at where some of them work in the control loop described above. See Figure 2.
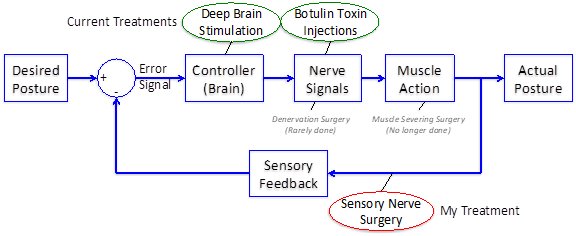
Figure 2 – Different dystonia treatments affect different parts of the neuromuscular control loop – Sensory Nerve Surgery is rare
Botulin toxins work by deadening targeted nerves within dystonic muscles. The point in the control loop where they work is highlighted in the control loop diagram in Figure 2. Thus, the nerve signals commanding the muscle into spasm are diminished and the muscle relaxes. Under this condition, nearby muscles that are less affected by ST (or unaffected) will do much of the work to maintain posture and move the body as desired. This is not quite natural, but it is far better than being frozen into one position by muscles in hard spasm.
Deep brain stimulation has been developed to implant small electrodes into the brain so that low-level electrical pulses can disrupt activity in the area around the electrodes. I am not knowledgeable in how these work, but I suspect they break up subconscious processes in the brain that lead to the over-stimulated nerve signals that result in muscle spasms. The area where this is likely working is also shown in Figure 2.
Two surgeries that are now rarely or no longer done are also shown. One is denervation surgery that removes the muscle nerves triggering the spasms. This is irreversible, so it is now rarely, if ever, done except in extreme cases where removal of specific nerves has been successful. The second involves severing of spastic muscles to eliminate the problem. This is no longer done because eventually the remaining muscles start going into spasm and the dystonic disabilities return.
In addition, various pharmaceuticals such as Clonazepam (the generic name of drugs like KlonopinTM) can help, too, and probably work by attenuating brain activity such that muscle commands are weakened and spasms are not a strong.
The part of the control loop diagram showing sensory feedback (circled in red) is where my treatment occurs. As described above, a damaged nerve deep within my left nasal passage triggers my ST. The damage to the nerve apparently sends corrupted nerve signals into the brain. The brain then interprets the signals as part of the sensory feedback and acts on them. In its effort to zero out the error signal, the brain erroneously commands muscles into powerful spasms. Since the corrupted signals do not change much, the posture that is induced by the spasms is persistent.
The sensory tricks I discovered helped by reducing pressure on and irritation of the nerve, which reduced the magnitude of corrupted nerve signals going into the brain. By reducing the severity of these corrupted nerve signals, the error signal is closer to the correct value. Consequently, the brain produces muscle nerve signals that allow better posture to be achieved. In addition, the topical analgesic applied deep within the nose further reduced unwanted nerve signals. Finally, the nasal surgery that shifted my septal bone away from the nerve reduced pinching and greatly reduced nerve malfunction.
Now What?
Since there are many ways within the brain that can result in severely incorrect nerve signals sent by brain to muscles, I doubt if sensory nerve damage can account for a majority of cases. But I suspect there are many such sensory nerve problems causing dystonia. These would be worth studying.
For example, in addition to the nasal nerve issue, the NSTA has become acquainted with dentists that specialize in Temporomandibular Joint (TMJ) disorders. The TMJ is the bone joint that the lower jaw pivots on. It is a heavily used joint (eating, speaking, etc.) and there is a sensory nerve that passes through it. The TMJ dentists (and now many doctors) have learned that many health problems can be caused by damage to the joint and the nerve passing through it, including some cases of dystonia. The dentists treat it with removable dental devices that the shifts a patient’s joint away from the damaged nerve. As with my nasal nerve, this relives pressure and irritation of the affected nerve and helps relieve the patient’s disorder.
One problem in the study of sensory nerves is that the body has an enormous number of them, and if one is damaged, it may not be apparent to the patient. If a patient cannot help a physician perform a diagnosis by pointing to an obvious problem, the physician may not know where to look because the damaged nerve may be remote from the symptoms. Remember, my damaged nasal nerve caused ST symptoms in my neck for about 40 years before I was able to track it down. That nerve only puts out a mild pressure sensation that is easily missed, even when I have no facial pain or muscle spasms to distract my attention. There has never been pain at the site of the damage. The corrupted nerve signals that were fed into my brain were apparently at a subconscious level leaving me unaware of the problem. The facial pain I lived with in parallel to the ST did not reveal anything about the nasal nerve, either. Nothing in the pain connected to the nasal region.
This is probably characteristic of many sensory nerve problems involved in ST. Defective nerve signals can be sent into the brain without pain, soreness, or other conscious signal being presented to the patient. Without this kind of information, medical science has to rely on that which can be measured and quantified. Deep brain stimulation is based on measurements of abnormally high brain activity. Botulin toxins are based on the well-know problem of botulism poisoning, which was known to kill by deadening nerves. Those who survived botulism then recovered nerve activity, so it was understood that if the pure toxin could be separated from the bacteria that made it, it could be a very good therapeutic for ST and other disorders. But sensory nerve disorders can be a hidden problem.
I will cover all of the above in my webinar on Saturday, January 15, 2022 at 1:00 p.m. Pacific Time and hope you join in. More of this topic will be covered, but since the subject is so complex I wanted you to have the opportunity to read about it first to be better prepared. You are encouraged to ask questions and talk a bit about any experiences you may have that suggest your ST is related to sensory nerve damage. If we start to find patients that can be treated by addressing sensory nerve damage, we may start a small revolution in ST care.
You are invited to a Zoom webinar.
When: Jan 15, 2022 1:00 PM Pacific Time (US and Canada)
Topic: Ken Price – My Unusual and Successful Treatment for my Spasmodic Torticollis (ST)
Register in advance for this webinar:
https://us02web.zoom.us/webinar/register/WN_G3fAFiIfSdukm4OUCVblfw
After registering, you will receive a confirmation email containing information about joining the webinar.

